Trusted by 100+ Practices & Medical Billing Companies

Why Your Practice Needs Automated Insurance Verification Software
Manual Eligibility Checks Lead to Denials
Up to 85% of claim denials are preventable, and eligibility errors are a primary cause. Each denial costs your team valuable time and money to rework. Veritable stops these errors before they happen, ensuring a higher clean claim rate.
Wasted Staff Hours Impact Revenue Cycle Management
Your front desk and billing teams spend hours each week on hold with payers or navigating clunky portals. Our software automates this tedious work, freeing your staff to focus on high-value tasks and patient care.
Inaccurate Data Creates a Poor Patient Experience
Unexpected bills are a leading cause of patient frustration. By providing accurate copay, deductible, and coinsurance data upfront, you create a transparent financial experience that builds trust and improves collections.
Meet Veritable, Your Complete Health Insurance Eligibility Verification Software Solution
Veritable was designed from the ground up to solve the real-world challenges of US healthcare providers. Unlike repurposed clearinghouse portals or clunky legacy systems, our platform is focused exclusively on providing the fastest, most accurate, and user-friendly eligibility verification experience. Whether you're a single provider or a high-volume billing service, Veritable is the software that scales with you.
Features of Our Insurance Eligibility Verification Software
Real-Time Eligibility Verification
Eliminate guesswork and administrative delays by checking patient insurance eligibility in real-time. Our platform connects directly to a comprehensive database of payers, providing you with accurate, up-to-the-minute coverage details before services are rendered. This proactive approach drastically reduces claim denials and improves the patient experience by providing upfront clarity on copayments and financial responsibility.
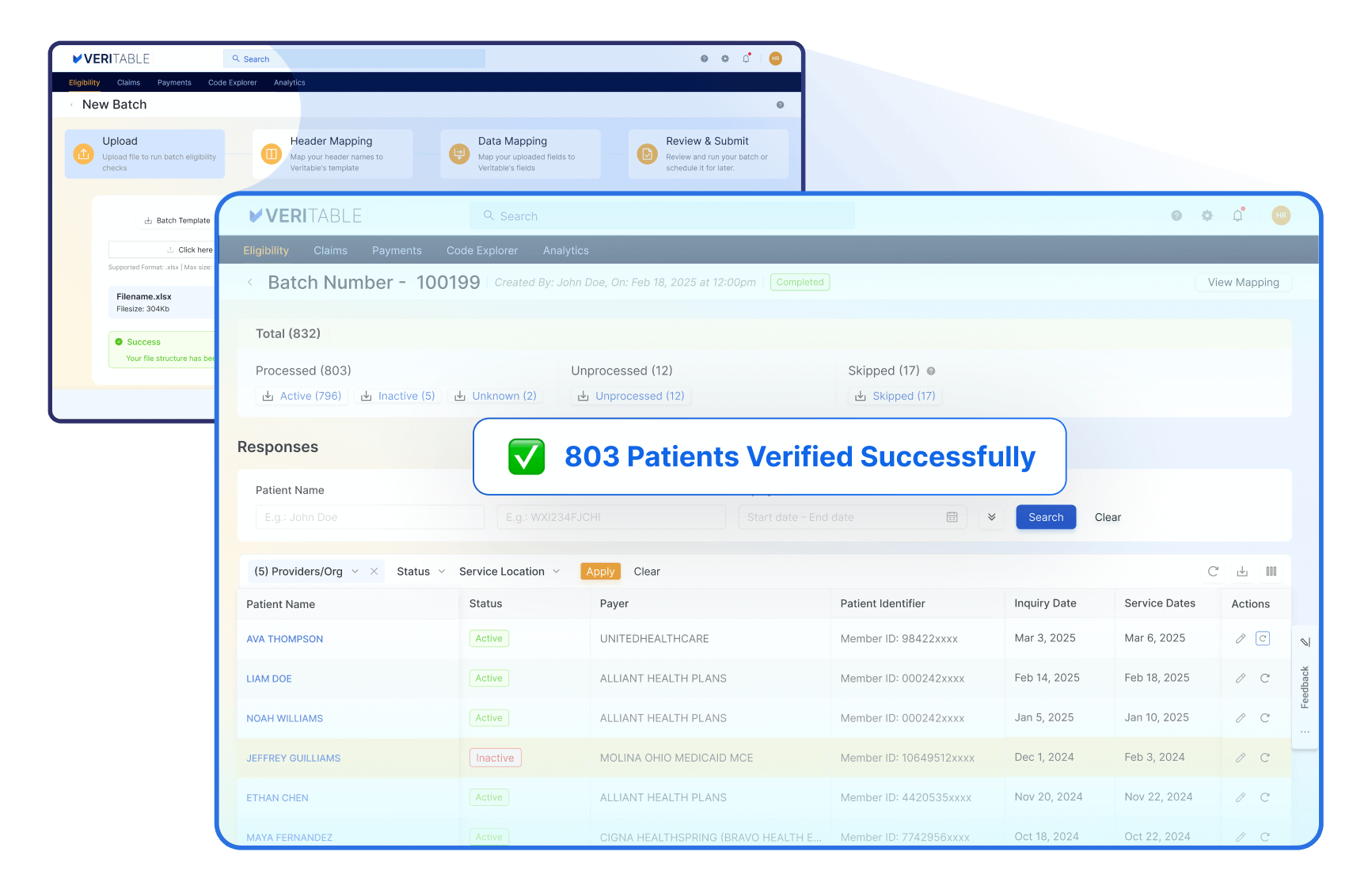
Self-Service Batch Upload
Effortlessly verify insurance for 100s of patients at once. Simply upload a CSV to automate checks across numerous payers, ensuring accuracy and drastically reducing manual data entry, all in just a few clicks.
Advanced Medicare, Medicaid & MCO Verification
Master the unique challenges of government payers. Our platform simplifies monthly Medicaid redeterminations, allowing you to upload and verify entire patient lists in bulk. When states change Managed Care Organization (MCO) partners, our software goes beyond a simple eligibility check to identify precisely which MCO is covering the patient. This ensures you always bill the correct entity, preventing costly errors and delays that commonly occur during these transitions.
Extensive Payer Network
Access our extensive network of over 1,000 commercial and government payers from a single connection. Eliminate the hassle of juggling multiple payer portals and logins, centralizing your entire verification process. This comprehensive coverage saves your staff valuable time and ensures you can confidently check eligibility for nearly any patient.
Flexible Service Type Checks
Go beyond a simple active/inactive status by verifying eligibility for specific service types. Our platform supports a wide range of specialties, including Medical, Dental, Vision, Mental Health, Chiropractic, and more. This granular detail ensures the services you provide are actually covered under the patient’s plan, preventing service-specific denials and providing greater financial certainty for your practice.
Transparent and Honest Pricing
We believe in transparent and honest pricing, without hidden fees or surprises. Our pricing structure is straightforward and designed to provide value for your investment. You can trust that our pricing aligns with the features and benefits that we deliver, allowing you to make informed decisions based on your practice's needs and budget. Get started for just $50, then pay only for what you use.
No-Cost Implementation & Training
Get started without any upfront investment in setup or training. Our dedicated team guides you through a seamless implementation process and provides comprehensive training to ensure your staff is confident from day one. We believe in a true partnership, which means we eliminate all hidden onboarding fees so you can see value immediately.
Streamlined Claim Status Check
Track the entire claim lifecycle from submission to reimbursement on one centralized platform. Gain immediate visibility into claim progress, empowering your team to proactively identify and resolve issues before they lead to denials. This direct oversight improves cash flow, minimizes payment delays, and reduces time spent on manual follow-up.
Flexible Data Export
Seamlessly integrate eligibility data into your other systems with flexible export options. We support industry-standard formats like FHIR and X12, as well as custom JSON, giving your technical team the power to build custom workflows and connect our data to your unique operational needs and analytics platforms.
Centralized Multi-Location Support
Effortlessly manage eligibility checks across all your practice locations from a single, unified account. This centralized approach simplifies administration, ensures consistent verification processes, and provides consolidated reporting, giving you a clear view of your entire organization’s performance without juggling multiple logins.
Scalable Team & Provider Management
Grow your practice without growing your costs. Our platform allows you to add unlimited providers (both NPI Type 1 and Type 2 organizations) and an unlimited number of users at no extra charge. Granular, role-based permissions ensure each team member only has access to the information and functions they need, safeguarding patient data and maintaining operational integrity as you expand.
Complete Audit & Usage Control
Maintain full visibility and control over your account activity. We provide detailed audit logs to track every action taken within the platform, ensuring compliance and accountability. With real-time usage monitoring, you can easily oversee your verification volume and operational trends, allowing for better resource management and cost forecasting.
Find Medical Codes Instantly
Access ICD-10-CM, ICD-10-PCS, HCPCS Level II, and CPT codes through a single, intuitive interface. Designed to reduce complexity, Code Explorer consolidates all essential code sets, making it easier to search, review, and apply the codes you need. With clear descriptions, structured hierarchies, and supporting guidelines, every lookup supports accuracy and informed decision-making.
Soc 2 Type II Compliant
We prioritize the security and confidentiality of your patient and practice data. We are SOC 2 compliant and implement stringent data security measures to protect against unauthorized access, breaches, or data loss. Rest assured that your sensitive information is safeguarded through industry-standard encryption protocols and regular security audits.
Prompt & Reliable Support
Never wait long for an answer when you need it most. Our knowledgeable support team is dedicated to resolving your questions and issues, with a guaranteed response within 24 business hours. This commitment ensures you can minimize operational disruptions and keep your practice running smoothly, backed by a team you can always count on.
User-Friendly and Intuitive Interface
Designed with simplicity in mind, Veritable offers an intuitive user interface that requires minimal training to use effectively. Accessible to both technical and non-technical users, our solution allows you to navigate effortlessly through various features and functionalities. Experience a smooth and user-friendly workflow that optimizes productivity and minimizes learning curves.
Cutting-Edge Technology
Our innovative healthcare product ensures accurate insurance eligibility verification and claim status checks. Built on a modern stack to ensure that you get real-time access to a comprehensive list of payers.
What Our Customers Are Saying
Simplified Pricing Based on Your Usage
Want to talk to us first? Let's schedule a call.
Veritable Is a Part of 314e Corporation
Like all 314e platforms, Veritable is backed by a dedicated support structure.
Founded in 2004 and headquartered in Silicon Valley, 314e Corporation delivers innovative, in-house–developed solutions across Revenue Cycle Management (RCM), Marketing Technology, Data Archival, Digital Adoption, Health Data Analytics, and Interface Engines. These products reflect our ongoing commitment to advancing healthcare technology.
Over the years, we have supported more than 250 hospitals across the United States. Our services span RCM, Epic consulting, EHR implementation, eLearning, training, interoperability, analytics, and IT services—enabling healthcare organizations to reduce costs while improving patient outcomes and experiences.
Get a Live Demo of Our Insurance Eligibility Verification Software
Schedule a personalized demo to see exactly how Veritable can fit into your workflow and start improving your revenue cycle right away.
Frequently Asked Questions
1. What is insurance eligibility verification?
Insurance eligibility verification is the process of confirming a patient’s active insurance coverage, plan details, and benefits before services are rendered. This includes verifying coverage status, copays, deductibles, coinsurance, and prior authorization requirements to reduce claim denials and improve billing accuracy.
2. What is an insurance eligibility verification software?
An insurance eligibility verification software automates the process of checking a patient’s insurance coverage, benefits, copays, deductible status, visit limits, prior authorization needs, and coordination of benefits (COB).
Instead of logging into multiple payer portals or calling payers manually, the software connects to payers electronically through HIPAA-standard EDI 270/271 transactions and returns consolidated, easy-to-read results in real-time.
This reduces administrative burden, accelerates patient intake, prevents claim denials, and ensures accurate patient cost estimates.
3. How does real-time insurance eligibility verification work?
Real-time eligibility verification sends an electronic request (EDI 270) to the patient’s payer and receives an instant response (EDI 271) showing current coverage and benefits. Modern software automates this process, delivering results in seconds and reducing manual steps like phone calls or portal logins.
4. Why is verifying insurance eligibility important before appointments?
Verifying eligibility ahead of time ensures the patient has active coverage for the services planned. It helps prevent claim denials, unanticipated patient liability, and staff workflow bottlenecks. Practices also use eligibility results to collect accurate copays and estimate patient responsibility before the visit.
5. What information is included in an eligibility verification check?
A typical verification includes:
✔ Active vs inactive status
✔ Coverage effective and termination dates
✔ Plan type (HMO, PPO, Medicare, Medicaid, etc.)
✔ Copay and coinsurance amounts
✔ Deductible and remaining balance
✔ Prior authorization needs
✔ Benefit limits and restrictions
✔ Coordination of benefits details (primary vs secondary)
This full benefit overview helps both clinical and billing teams manage patient accounts with confidence.
6. How does insurance eligibility verification reduce claim denials?
Automated verification catches coverage gaps, inactive policies, missing authorizations, and benefit limitations before claims are submitted. By identifying these issues early in the patient intake or scheduling process, practices can fix errors upfront, resulting in fewer rejections and faster reimbursements.
7. Does eligibility verification software support Medicaid and Medicare?
Yes, modern solutions typically support Medicare (Parts A/B/Advantage), Medicaid (state and managed plans), commercial insurance, and often dental/vision plans. Real-time software connects to these payers to confirm active eligibility and benefit details.
8. Can software check multiple patients at once?
Yes. Most eligibility verification tools offer batch verification, enabling practices to check eligibility for dozens or hundreds of patients in a single upload or automated workflow, saving hours of manual work.
9. Will the software integrate with my EHR or practice management system?
Yes, leading insurance eligibility verification software integrates with many EHRs and PM systems (Epic, Athenahealth, NextGen, eClinicalWorks, etc.), so verified coverage results flow directly into the patient record or billing workflow.
10. How quickly will I get eligibility results?
With real-time systems, results typically return in seconds for single checks. Batch uploads for very large lists may take a few minutes, depending on the volume and payer response times.
11. Is eligibility verification software HIPAA compliant?
Yes. Legitimate solutions adhere to HIPAA standards for protected health information, ensuring encryption, secure transmissions, and audit logging, which protect patient data and support compliance requirements.
12. Who Needs Insurance Eligibility Verification Software?
This solution creates immediate efficiency for:
- Primary care practices
- Specialist practices (Ortho, Cardio, Oncology, Ortho, GI, etc.)
- Multi-specialty groups
- MSOs + DSOs
- Behavioral health providers
- Surgery centers (ASCs)
- Hospital outpatient departments
- Telehealth providers
- Diagnostic centers
- Physical therapy + rehab centers
- Revenue cycle and billing companies
Any organization that deals with insurance billings will save time and reduce denials with automated eligibility verification.