Trusted by 100+ Practices & Medical Billing Companies

Where Is Your Revenue Leaking?
At Patient Check-In
Every patient with unverified or inaccurate insurance is a potential revenue leak. These small drips: denials, rejections, and write-offs accumulate into a significant financial drain on your practice.
In Your Administrative Workflow
Operational drag from manual phone calls and navigating complex payer portals ties up your most valuable resource: your staff. This inefficiency not only costs you money but also leads to burnout and diverts focus from patient care.
During Patient Collections
When coverage is a question mark, so is patient responsibility. This uncertainty leads to difficult financial conversations, surprise bills, and a higher rate of uncollected balances, eroding both revenue and patient trust.
Veritable - Your Proactive Partner for Insurance Eligibility Verification Services
Our insurance eligibility verification services are designed to seal these leaks for good. Veritable acts as an automated checkpoint at the very start of your revenue cycle. By delivering instant, crystal-clear benefits information directly into your workflow, we empower your team to prevent problems before they start, transforming a reactive process into a proactive strategy for financial strength.
How Our Insurance Verification Services Empower Your Practice
We provide a comprehensive service experience, combining powerful technology with the support you need to succeed. This is how we empower your team at every step:
Verify Eligibility in Real-Time
Veritable connects directly to a comprehensive database of payers, providing you with accurate, up-to-the-minute coverage details before services are rendered. This proactive approach eliminates guesswork, drastically reduces claim denials, and improves the patient experience by providing upfront clarity on financial responsibility.
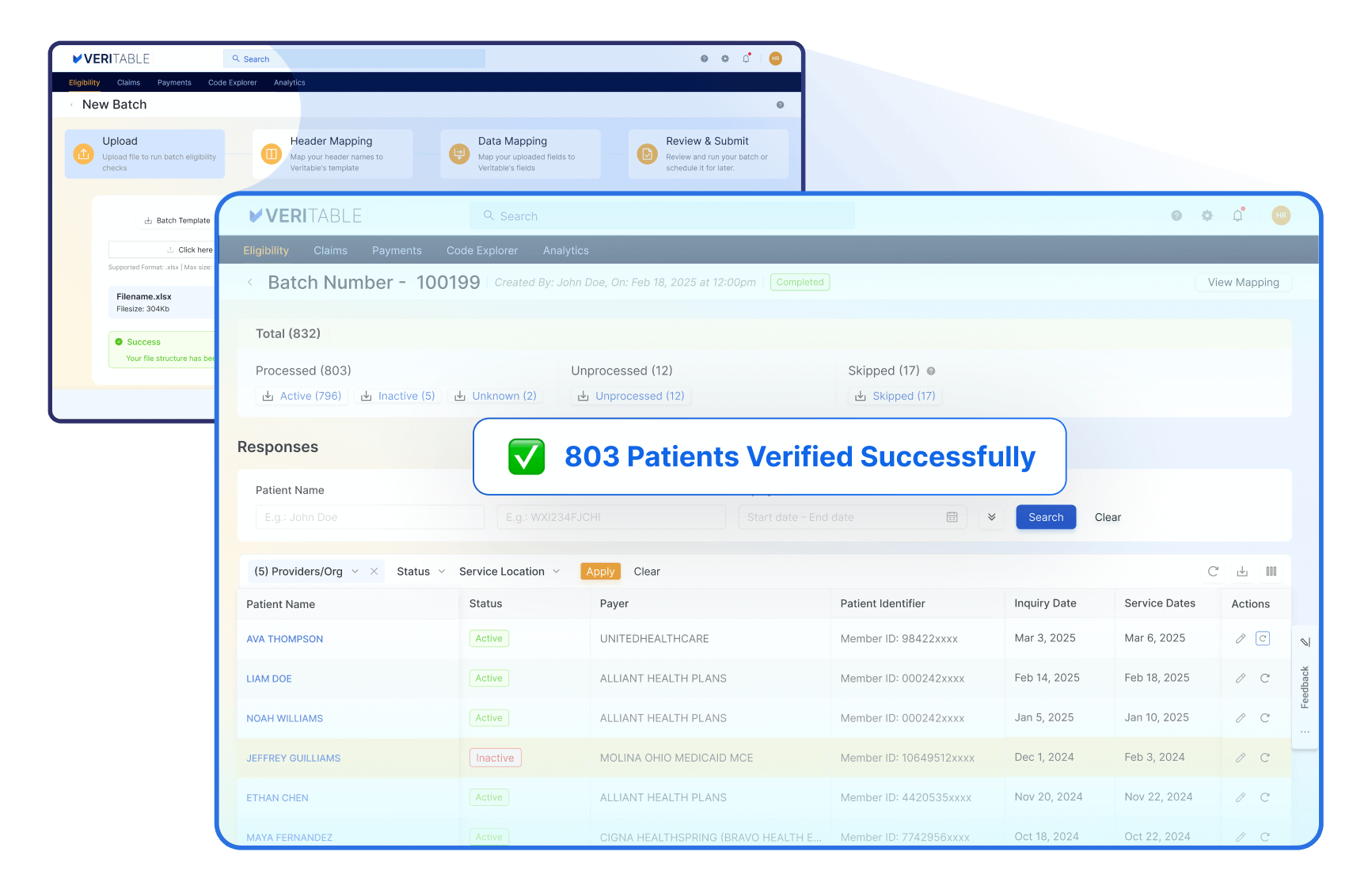
Enable Effortless Batch Verification
Our Self-Service Batch Upload empowers you to verify insurance for hundreds of patients at once. Simply upload a CSV, and our service automates checks across numerous payers, ensuring accuracy and drastically reducing manual data entry for your entire next-day schedule.
Master the Complexities of Government Payers
Our platform provides precise verification for Medicare (including Part A/B status) and simplifies monthly Medicaid redeterminations. When states change Managed Care Organization (MCO) partners, our software identifies exactly which plan is covering the patient, ensuring you always bill the correct entity and prevent the costly delays common with government insurance.
Connect to a Vast Payer Network
Access our comprehensive network of over 1,000 commercial and government payers from a single connection. Eliminate the hassle of juggling multiple payer portals and logins by centralizing your entire verification process. This broad coverage saves your staff valuable time and ensures you can confidently check eligibility for nearly any patient.
Ensure Coverage for Specific Service Types
Go beyond a simple active/inactive status by verifying eligibility for specific service types. Our platform supports a wide range of specialties, including Medical, Dental, Vision, and Mental Health. This granular detail ensures the services you provide are actually covered, preventing service-specific denials and providing greater financial certainty.
Build Your Budget on Transparent Pricing
Building a partnership requires trust. We believe in transparent and honest pricing, without hidden fees or surprises. Our straightforward structure, with subscriptions starting at $50 and additional usage billed on a pay-as-you-use basis, is designed to provide clear value for your investment, allowing you to make informed decisions that fit your practice's budget.
Start With Zero-Cost Implementation & Training
A true partnership means investing in your success from the start. Our dedicated team guides you through a seamless implementation process and provides comprehensive training to ensure your staff is confident from day one, all at no extra cost to you.
Track Every Claim, On-Demand
Gain immediate visibility into your revenue cycle by tracking the entire claim lifecycle from submission to reimbursement on one centralized platform. Veritable empowers your team to proactively identify and resolve issues before they lead to denials, improving cash flow and minimizing time spent on manual follow-up.
Integrate Your Data With Flexible Exports
Seamlessly integrate eligibility data into your other systems with flexible export options. We support industry-standard formats like FHIR and X12, as well as custom JSON, giving your technical team the power to build custom workflows and connect our data to your unique operational needs.
Manage All Your Locations From One Place
Effortlessly manage eligibility checks across all your practice locations from a single, unified account. This centralized approach simplifies administration, ensures consistent verification processes, and provides consolidated reporting, giving you a clear view of your entire organization’s performance.
Scale Your Practice Without Extra Fees
Grow your practice without growing your costs. Our service allows you to add unlimited providers (both NPI Type 1 and Type 2 organizations) and unlimited users at no extra charge. Granular, role-based permissions ensure each team member only has access to the functions they need, safeguarding data as you expand.
Provide Your Team With a Simple Interface
Designed with your workflow in mind, our platform offers an intuitive user interface that requires minimal training. Both technical and non-technical users can navigate effortlessly through features, optimizing productivity and ensuring a smooth workflow from day one.
Safeguard Your Data With Uncompromising Security
We prioritize the security of your patient and practice data. As a SOC 2 Type II compliant organization, we implement stringent security measures, including industry-standard encryption and regular audits, to protect against unauthorized access. You can have peace of mind knowing your sensitive information is always protected.
Get a Partner in Your Success
Our commitment doesn't end after setup. We pride ourselves on providing exceptional, reliable support throughout your journey with us. Our knowledgeable and friendly team guarantees a response within 24 business hours, ensuring you always have a partner to count on.
See the Impact on Practices Like Yours
Simplified Pricing Based on Your Usage
Want to talk to us first? Let's schedule a call.
Veritable Is a Part of 314e Corporation
Like all 314e platforms, Veritable is backed by a dedicated support structure.
Founded in 2004 and headquartered in Silicon Valley, 314e Corporation delivers innovative, in-house–developed solutions across Revenue Cycle Management (RCM), Marketing Technology, Data Archival, Digital Adoption, Health Data Analytics, and Interface Engines. These products reflect our ongoing commitment to advancing healthcare technology.
Over the years, we have supported more than 250 hospitals across the United States. Our services span RCM, Epic consulting, EHR implementation, eLearning, training, interoperability, analytics, and IT services—enabling healthcare organizations to reduce costs while improving patient outcomes and experiences.
Secure Your Revenue Cycle Today
Let's start a conversation about your practice's financial health. Schedule a brief, no-obligation demo and see how Veritable’s healthcare insurance eligibility verification services can make your revenue cycle stronger and more predictable.
Frequently Asked Questions
1. What is insurance eligibility verification?
It is the process of confirming a patient’s active insurance coverage, benefits, and financial responsibility before services are provided.
2. Why should I automate eligibility verification?
Automation eliminates manual errors, reduces denials, and speeds up patient access — saving time and improving revenue cycle performance.
3. What information is checked during eligibility verification?
Coverage status, benefits, deductibles, copay, coinsurance, COB, authorization requirements, service limits, and payer-specific rules.
4. What is real-time eligibility verification?
It refers to instant EDI 270/271 checks that return benefit data in seconds for any patient.
5. How does secondary or tertiary insurance detection work?
The system queries payers for all active coverage layers and identifies additional insurance linked to the patient.
6. Does eligibility verification guarantee payment approval?
No, it confirms coverage and benefits, but payment still depends on medical necessity, coding, and claim accuracy.
7. How fast are eligibility results returned?
Veritable processes real-time eligibility checks in seconds.
8. Can Veritable integrate with my EHR or PMS?
Yes, we offer API, HL7/FHIR, and SFTP integrations for seamless workflow embedding.
9. How accurate are the results?
Our system uses advanced benefit parsing, payer rule logic, and quality checks to ensure highly accurate data output.
10. Is Veritable HIPAA compliant?
Absolutely. All data is encrypted, audited, and processed per HIPAA and SOC 2 requirements.